Abstract
BACKGROUND
Household demographic and socioeconomic status (SES) variables have been demonstrated to influence treatment decisions and outcomes across a wide range of health disciplines. The relationships between factors such as race, marital status, work status, type of residence, income, insurance payer, and outcomes following allogeneic hematopoietic cell transplantation (alloHCT), however, have not been clearly elucidated. To maximize the likelihood of success, it is essential to determine the impact of these factors so that additional resources can be targeted to at-risk patients. Those who survive the initial alloHCT period remain at risk for long-term complications, thus the ability to align post-transplant support with specific patient needs may influence survival outcomes.
METHODS
This retrospective single center study evaluated demographic and outcome data for all consecutive patients who received an alloHCT at the University of California, San Francisco (UCSF) between January 2012 and January 2016. SES data were obtained from social work evaluations conducted prior to and after alloHCT. ZIP codes of primary residence were linked to median household income using 2010 Census data. Using this income data, patients were divided into surrogate income quartiles, with the top quartile earning ≥$89,811 annually and the bottom quartile ≤$50,222 annually. Primary endpoints included relapse free survival (RFS), overall survival (OS), and non-relapse mortality (NRM).
RESULTS
During the period of study, 269 patients underwent alloHCT. Median followup was 2.1 years (yrs). Amongst transplant recipients, 175 (65.1%) were Caucasian, 48 (17.8%) were Hispanic, 37 (13.8%) were Asian or Hawaiian/Pacific Islander, and 9 (3.3%) were African American. Matched related donors were used for 103 (38.3%) patients, unrelated donors for 149 (55.4%), haploidentical donors for 11 (4.1%), and umbilical cord blood for 6 (2.2%). The median age at time of alloHCT was 54 years (range 20-76 yrs). Myeloablative conditioning was used in 143 (53%).
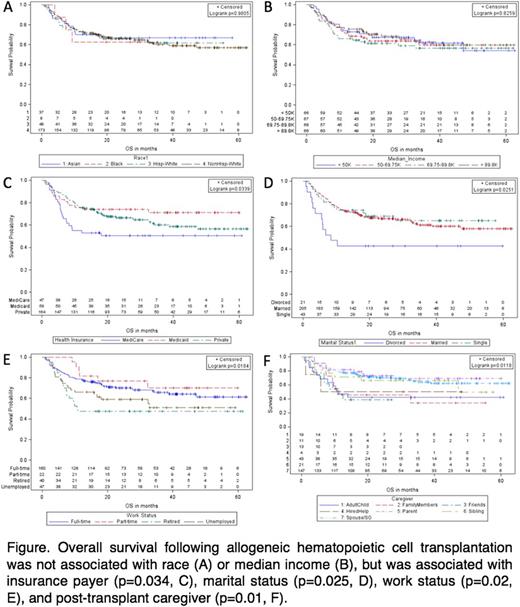
In this cohort, RFS was not associated with race, marital status, work status prior to alloHCT, income, caregiver, type of residence after transplant, distance from medical center, or insurance payer. OS was not associated with race, type of residence, distance from medical center, or income. The insurance payer Medicare was associated with decreased OS in comparison with patients whose payer was Medicaid (state payer) or private insurance (p=0.034), but this finding is confounded by age (median age 67, 37, and 53 yrs, respectively). There was no significant survival difference between those with Medicaid or private insurance. Retirement status prior to alloHCT also correlated with decreased OS in comparison with those with full-time, part-time, or no employment (p=0.018). Being divorced was associated with decreased OS in comparison with those who were single or married (p=0.025). The primary designated caregiver was significantly associated with OS, with those having a spouse, parent, or sibling caregiver having prolonged survival in comparison with those whose caregiver was an adult child, other family member, friend, or hired aid (p=0.012). Based on estimated household income, the top income quartile had significantly lower risk of NRM (4.3%), compared to the upper middle (15%), lower middle (11.6%), and bottom (11.9%) quartiles (p= 0.048). NRM was not associated with the other variables assessed. Acute GVHD (overall and grade 2-4) and chronic GVHD incidence rates were not associated with the SES variables assessed.
CONCLUSIONS
We found that SES variables do not influence relapse rates, suggesting relapse risk is primarily driven by factors intrinsic to the indication for transplant, as expected. Most of the social variables we assessed also were not associated with OS after alloHCT. Insurance payer and retired status prior to alloHCT were associated with decreased OS, but both of these variables are confounded by age. Importantly, divorced relationship status and caregivers who were adult children, friends, hired aids, or family members other than a spouse, parent, or sibling were significantly correlated with decreased OS. Our findings have the potential to influence recipient risk stratification, housing and caretaker requirements following transplant, and the provision of means-based assistance for at-risk individuals.
Mannis: Curis: Honoraria; Juno: Research Funding; Amgen: Honoraria; Agios: Research Funding. Logan: Incyte: Consultancy; Jazz: Consultancy; Kite: Research Funding; Shire: Consultancy; Pharmacyclics: Research Funding; Astellas: Research Funding; Novartis: Consultancy, Research Funding; Amgen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal